Chapter 4: Health and Aging
Learning Objectives
After reading through Chapter 4: Health and Aging, students should know, learn, or be able to do the following:
- Analyze Health-Aging Dynamics and Indicator Decreases: Analyze the intricate connection between health and aging, exploring how diminishing health indicators over time contribute to the aging process, and critically evaluate the implications of these changes on individuals’ well-being.
- Evaluate Human Health Warranty and Age-Related Susceptibility: Evaluate the concept of Human Health Warranty, assessing its implications on human susceptibility to health-related issues as age advances, and apply critical thinking to discuss potential strategies for managing these challenges.
- Examine Physical Changes with Aging: Examine physical changes, including alterations in hair, skin, and body composition, that occur as humans age, and critically assess how these changes impact self-perception and societal attitudes toward aging.
- Analyze Sensory and Perception Alterations: Analyze the diverse sensory and perception changes that accompany human aging, including vision, hearing, balance, taste, smell, touch, and pain, and evaluate the potential consequences of these changes on individuals’ daily lives.
- Assess Vital Bodily Function Changes and Implications: Assess the changes and degradation in vital bodily functions as humans age, including incontinence, hypothyroidism, decreased immunity, and altered sleep patterns, and compare and contrast the implications of these aging symptoms on overall well-being.
Chapter Outline
- Human Health Warranty
- Conceptualizations of Health
- Normative Biological Changes
- Vital Bodily Functions
- References
Americans live to breathe. This had become a commonly adopted and socially accepted worldview of health. Our individual health is extremely important and priceless. Yet, some adults maintain the belief that “you only live once (YOLO)” and thus they tend to be careless when it comes to protecting health. Such individuals tend to engage in risky health behaviors such as smoking, binge drinking alcohol, consuming large amounts of high sugar and high caffeinated energy drinks, staying awake all hours of the night and functioning on less than six hours of sleep, or engaging in unprotected sexual intercourse. On the other hand, a growing proportion of individuals expressed a heightened awareness about their health and prefer to protect and maintain health functioning for as long as possible across the course of their adult human life-span and into old age. Many of these adults will visit a physician for a routine annual physical, periodically check key vital signs such as temperature, blood pressure, respiration, and pulse, or even opt to order the salad or vegetarian menu item over the usual cheeseburger, fries, and large soda at the drive-thru. Meanwhile, others spend countless amounts of time and energy going to the gym, hitting the weights, exercising, and staying fit in order to maintain peak levels of strength and performance. Furthermore, many adults remain food conscious and highly attentive and aware of the nutritional content of the food they consume by checking the caloric content, type and amount of fat, percent of sugars and added sugars, and overall ingredient listing on printed labels of food products which they purchase to eat, drink, and ingest and absorb into their bodies.
Health is way of life in today’s contemporary world. Any given second, minute, hour, or day we are bombarded by marketing advertisements on television, radio, podcasts and webpages, that claim to delay, prevent, or eradicate aging in some way, shape, or form. You are not alone if you have experiment with the latest exercise, diet or health craze, purchased an anti-aging beauty product, or consumed the latest designated “super food” which marketed and advertised as helping humans look, feel, and be younger. Countless number of persons have fallen victim to spending money on skin care lotions and products, fruit and vegetable-based energy drinks, pills, vitamins and protein powders; smart watches and other devices, trinkets, and whatnot, that promise to enhance immunity, ward off disease, and make it easier live a longer and healthier life. Why would not a person try such products from time-to-time? For centuries, we humans have possessed a certain a level of curiosity when it comes to seeking and discovering the fountain of youth and eternal health. Even Ponce de León, the great Spanish explorer, led an expedition along the coast of Florida in 1513, where myth and legend suggests he discovered the fountain of youth in what is now the community of St. Augustine, the oldest continuously occupied European settlement and city in the United States. Here, Ponce de León claimed he had discovered magical healing waters which restored one’s youthful appearance, vigor, and stamina. Unfortunately, de León’s life was cut short when he was wounded by an arrow in his thigh during a skirmish with the native Calusa people while attempting to establish a Spanish colony in Southwest Florida. De León died from his wounds, likely due to his body’s inability to fight infection, a few months later. An ironic twist of fate in the fountain of youth myth which has persisted for over 500 years. Nonetheless, our health is the ultimate investment with the greatest lifetime of potential return. If we do not make attempts to seek, discover, or invest in our health, then the probability that we will succumb to disease, disablement, or death before rather reaching a successful old age will increase.
Human Health Warranty
When does human health begin to fail? Some experts contend that mid-life marks the beginning of the end of the human health warranty, or the state in which the human species can expect to encounter biological loss and physiological constraint that necessitate medical intervention and monitoring in order to sustain continued functioning and delay mortality. Carnes and Witten (2014) revealed that the chronological age period of 50-55 years represents the effective beginning of biological decline and increased susceptibility to disease and disablement in humans. Three processes are hypothesized as effectively changing our biological system between the 50-55 year age period. For women, age 50 typically marks the beginning of menopause, or the cessation of the menstrual cycle and end of reproduction. In fact, the average age of menopause is around 51 years of age. There are three stages of menopause. First, there is perimenopause which can occur 3-5 years before menopause. When women reach their late 40’s, estrogen and hormonal levels begin to drop which contributes to irregular menstrual cycles and a variety physical symptoms that can include: hot flashes, insomnia, night sweats, elevated heart rate, mood disturbances, vaginal dryness, and urinary problems. Menopause represents the second stage. Menopause technically occurs when a woman has missed their period for at least 12 straight months without experience of illness, medication, pregnancy or breastfeeding. The transition from perimenopause to menopause can take an estimated 1-3 years. The third stage involves post-menopause. Post menopause begins one year since the last menstrual cycle of period. Similar to periomenopause, it is not unusual to experience the aforementioned physical symptoms. Continued decreases in estrogen during this stage put women at greater risk for increased health risks including weight gain, heart disease, and osteoporosis. It is important to note that events other than normative aging do contribute to an earlier menopause. For instance, women that undergo surgical removal of the uterus or hysterectomy will certain experience an early menopause than their counterparts who do not.
On the other hand, middle aged men after age 50 may experience a process referred to as andropause. This is often referred to as “male menopause” and is largely used to describe decreasing testosterone levels. However, it is important to note that this process is significantly different from women. In women, ovulation ends and hormone production diminishes in a relative short period of time. Among men, the production of testosterone and other hormones gradually declines at a much slower rate and elongated period of years, and many men experience no symptoms whatsoever. Most older men are able to maintain testosterone levels within the normal range. In fact, there is much variability among those who have levels considered low with an estimated 10-25% of men considered to have low testosterone. Unlike women experiencing menopause, men can also remain fertile well-beyond 50 years of age and across the entirety of their life-span. Yet, experts note that aging men normatively have negative semen and fertility parameters that can contribute to difficulty reproducing with a partner, as well as greater risk of offspring born with physical or neurological health problems (Mazur & Lifpshultz, 2018). That being said, it is still not well-understood whether the symptoms men report are due to low testosterone or other normative age-associated health conditions linked to a high body max index or increase use of certain prescriptions medications. Nonetheless, common signs and symptoms of adndropause can include things such as:
- Increased weight gain and body fat
- Complaints of fatigue or low energy
- Reduced libido or sexual desire and activity
- Hot flashes and sweating
- Low bone mineral density
- Erectile dysfunction
- Sleep disturbances and insomnia
- Depressed mood
- Reduced sperm count and fertility
In 2018, the Endocrine Society recommended testosterone therapy for men with age-related signs and symptoms of low testosterone. However, further research is needed to determine the negative effects of such treatment. Such treatment can increase risk of stroke, heart attack, and blood clots in men. Thus, it is always best for men to consult a physician before deciding to be placed on any type of testosterone therapy.
In addition to the effective end of reproduction, sex ratio differences also warrant concern relative to a health warranty period. Sex ratio pertains to the available pool of prospective reproductive mates. The highest risk of from avoidable mortality occurs around the age of sexual maturity or approximately age 25 through age 35. There is evidence that number of males and females born during any calendar year can vary. Nonetheless, there has historically been a greater number of females born with the exception of greater equality in sex ratio which had occurred since the 1970’s. This may be explained by the (1) absence of major world wars, such as World War II and the Vietnam War, during which a greater number of sexually mature men were killed and are effectively taken out of the mate selection pool, as well as, (2) more recent advances in medicine and health care that have improved and benefited life expectancy of males more than females (Carnes & Witten, 2014). Thus, human life histories can impact the health warranty by the fact of reproductive biology and the failure or ability to pass on genetic qualities that afford men and women a warranty extension, whereby 50-55 years may be a plausible window of time.
A final contributing factor to the health warranty involves mortality. Risk of mortality exhibits a significant acceleration for both males and females after age 50. In other words, with each additional year of life lived after 50 years, humans have an significantly reduced chance of survival to live another year. The longer we continue to live the more accelerated is our chance for mortality. The only thing standing in-between human survival and the threat of death after age 50 is the fact that many of us will routinely engage in preventative health screenings, seek diagnositic testing for abnormal health symptoms, and undergo minor and major surgical procedures as a corrective cure. In other words, human interaction with modern medicine after age 50 helps to extend an expired warranty. Thus, reaching the end effective end of one’s human health warranty is not an automatic death sentence, yet it is important to know that the morbities, or rate of acute, chronic, and lethal diseases, that can impede our health performance and eventually lead to our death start to accelerate the process toward death. According to Carnes and Witten (2014), there is a fourfold increase in lethal morbidities by age 55; a 12-fold increase by age 65; and a 40-to 50-fold increase by age 80. Thus, human need to prepare for geriatric health prevention in their 50’s rather than wait until a later age for continued health survival.
Conceptualizations of Health
You may be asking yourself, what basic types of morbities or health conditions might I encounter once I reach middle age and cross the threshold into late adulthood? For starters, health can be divided in to three simple types. First, there is a physiological health type. Physiological health relates to the body’s ability to physiologically function and is best demonstrated by varying health systems such as the cardiovascular, circulatory, respiratory, musculoskeletal, and nervous system. Physiological health is best assessed and evaluated through objective means or tools designed to produce a numerical marker, range, or some other indicator reflective normative versus below normal function. Vital readings are a good example and include objective physiological assessments in the form of weight and height, thermometer readings for body temperature, blood pressure, pulse rate, and respiration rates. More sophisticated ways of evaluation come in the form of blood testing and comparison of white versus red blood cell counts, levels of detectable sugar or iron in the blood, and other comparable tests. Such assessments allow for a determination of whether our physiological health is functioning at a normative level or may be operating under stress depending on what the objective numerical indicator may be and where it may fall on the continuum of normality. Second, there is the functional health type. Functional health relates to the individual ability to engage in some type of physiological function relative as demonstrated through the observation of kinesics or movement and mobility. Of particular importance is the observing performance related to how well one is one is able to move their arms and legs, walk, and perform daily tasks vital to one’s livelihood, health, and well-being. Functional health is usually evaluated in one of two performance areas:
- Physical Activities of Daily Living (PADLs), or everyday task that require performance of routine coordination of movement in the form of sitting, standing, walking, as well as, getting in and out of bed, being able to get on and off a toilet, feeding oneself, and putting on and taking off clothing
- Instrumental Tasks of Daily Living (IADLs) or daily performance of tasks requiring routine minor movements but essential to one’s well healthy well-being including shopping, cooking, operating and driving a vehicle, taking over-the-counter or prescription medication, paying the bills and monitoring finances, or vacuuming or cleaning one’s living area.
A third and final type of health pertains to perceived health, or subjective and qualitative judgement of how one may physically or functionally feel or rate their current state of health. It is not uncommon for humans to base their subjective or qualitative report of health based on social comparison. In fact, older adults commonly compare their health to same-age peers and often report feeling or looking younger, better able to accomplish everyday tasks of living, and physically healthier. Some experts contend that social comparisons of health may actually benefit and protect older adults from developing a negative self-perceptions about their health (Cheng & Chan, 2007; Sayag & Kavé, 2022); thus allowing them to worry less about minor acute symptoms yet pay attention to more significant health problems that might arise. Over time, self-rated perceptions of health tend to be helpful predictors of impending morality among middle aged and older adults (Lorem et al., 2020; Wuorela et al., 2020)
Normative Biological Changes
Physical and Bodily Appearance
How do you know someone is old? Most likely, the first thing that comes to mind are physical features such as wrinkles and gray hair. These are some of the most commonly recognized physical signs of change in our human biology. Humans tend to judge the maturity or age of others on the basis of appearance. There association between the physical signs of aging and the latent changes occurring within the body is often mixed, yet some experts believe that what can be seen on the outside is often an indication of what is likely happening on the inside when it come to human aging (Blume-Peytavi et al., 2016; Christoffersen & Tybjerg-Hansen, 2016).
Skin
Our skin is the largest organ in the human body. Our skin undergoes a visible transformation reflecting age-related changes as early as the 20’s with the first signs of aging appearing in our 30’s. By the time persons reach age 50, changes in the skin are most apparent around our face, hands, feet, and upper arms. Age-associated changes occur across the various layers of the skin starting with the epidermis, or the outermost layer of skin. The epidermis consist of a thin layer of cells protecting underlying tissue, which loses integrity and patterning with advancing age. The dermis is the middle layer of skin that lies just under the epidermis. The dermis consists of connective tissue, in which nerve cells, glands, and hair follicles. Changes in collagen and elastin, two key protein molecules contribute to changes in the dermis. First, cross-linking of the collagen molecules causes the skin to become more rigid and less flexible. Meanwhile, elastin, a molecule that promotes skin flexibility, is less able to return back to its natural shape as one ages. As we reach mid-life and beyond, this leads to a sagging appearance of the skin particularly around the arms, neck, and face. Below the dermis lies the subcutaneous layer of skin, or the most bottom layer which give the skin its opacity smoothing the curves of our arms, legs, and face. Around middle age, this layer begins to thin and provides less support for the other layers above it. Promote features of this process include increased wrinkling and sagging of the skin. Another prominent feature involves the appearance of visible blood vessels just beneath the skin.
Human skin changes color over the course of our adult life and into old age. A common visible sign of skin aging involves the appearance of lentigo senilis, or age spots, which appear as areas of brown pigmentation particularly on sun-exposed portions of our skin such as the face, hands, arms, and legs. Fair-skinned persons are especially vulnerable relative to developing age-spots over their life-span. Furthermore, it is fairly common for persons to also develop and increasing number of pigmented outgrowths such as moles, as well as angiomas or visibly elevated blood vessels.
Our nails are also a part of skin subject to normative age-associated changes. Our toenails grow more slowly as we age, as well as develop a yellowed and rigid thickened appearance. Many older adults develop fungal infections in their toenails. This causes the nails to thicken and separate from the nail bed. Yeast, bacteria, and molds can also contribute to nail infections. For instance, bacterial infections of the nails is usually visible as a green or black discoloration of the nail. Key risk factors include older age, diabetes, circulatory problems, psoriasis, walking barefoot around damp or wet areas, and wearing shoes that cause the feet to sweat heavily. Medications that suppress the immune system can also make older adults more suspectibl to fungal issues of the nails. In severe cases, fungal infections of the toenails can be painful, lead to permanent nail damage and require removal of the toenail.
General changes to the skin further exacerbate changes in the physical appearance of the face. There are normative changes relative to bone loss in the skill, as well as cartilage changes of the nose and ears, resulting in the nose and ears becoming elongated. In addition, our facial muscles lose the ability to fully contract, thus resulting in diminished smiling width (Chetan et al., 2013). Such changes in our physical facial appearance can make it difficult for others to determine whether we may be happy and content or sad and upset.
Our genetics plays a large part in how slow or fast our skin ages. Fair-skinned persons tend to display a more rapid rate of aging of the skin compared to those with darker or olive-complicated skin. In addition, lifestyle behaviors which increase exposure to sunlight, such as working outside, sun bathing, or driving with the top down, can significantly accelerate the rate at which our skin ages. This is primarily due to photoaging, or age-related changes in the skin due to exposure to ultraviolet light from the sun which accelerates cross-linking, causes mutations altering protein synthesis, and increases production of free radicals.
Hair
Beyond the appearance of skin, our hair represents one of the most outward visible signs that the body is aging. Hair itself does not turn gray; rather the number of pigmented or colored hairs on our head decreases while the number of non-pigmented hairs on our head increases. Around 50 years of age, the production of melanin, which gives our hair color, slows and eventually stops being produced. By the time persons reach 75-80 years of age, there are no naturally colored hairs left on the scalp or other areas of the body. The natural color of our hair no longer exists, and thus we remain gray haired for the remainder of life.
Along with diminished pigmentation, both men and women can expect to experience loss and thinning of the hair. This tends to be more pronounced and visible in men and is a results from the destruction of the germination centers responsible for producing growth of hair in the hair follicles. Although there are several types of hair loss linked to immunity imbalances (areata), stress from childbirth (telogen), radiation/chemotherapy (anagen), and thermal hair treatment damage (traction) the most common type impacting older adults is androgenetic alopecia (see photo insert), in which long, thick, and pigmented hair or terminal hair is no longer produced and instead is replaced by short, fine, unpigmented hair or vellus hair, which is largely invisible. This type is typically linked to genetics and hormonal changes in aging. For men entering mid-life, it usually comes in the form of male-patterned baldness in which the hairline gradually recedes of moves backward in the form of a “M” shape, while a circular area on the back of the head may thin or gradually expand. Typically, this process results in hair no longer growing on top of the head. Instead, most older adults will find that hair continues to grow and appear in thicker amounts in places on the head where it is not necessarily wanted, such as ones’ chin, ears, or eyebrows. There is no cure to end gray hair or thinning and baldness, but consumer topical hair shampoos such as Rogaine can certainly simulate some hair growth; whereas hair coloring beauty products can reduce some depigmentation.

Body composition
When it comes to the physical maturity, shape, and size of the human body during the middle adult years, most persons experience change in the form of a different resemblance than when they were younger. You may have heard many middle-aged adults refer to this change as the middle age “bulge” or “spread.” By the time persons reach 50-60 years of age, one of the first things they will notice is a redistribution of fat in different parts of the body, which creates a new body build or look. Most persons will notice an accumulation of fat resulting in a wider waist and hip circumference. Yet, there is a clear explanation for this process and why it seems more noticeable during our middle years. First, there is conclusive research evidence that people get shorter as they get older. It is a fact. We shrink in height with age. Human can expect to lose nearly one-half inch in height every 10 years after age 40. By the time persons reach 70 or more years of age, it not unusual to lose a total of 1 to 3 inches in height. Normative age-associated height decrease tends to be more accelerated and pronounced for women. Loss in height over time is due to normative aging processes linked to loss of bone mass in the vertebrae, which results in spinal collapse and a shortening in length (Kaiser et al., 2018). Another explanation for why our bodies change in size and stature involves normative loss in lean body tissue and muscle or what is referred to as fat-free mass (FFM). This contributes to changes in our overall body composition, or body mass index (BMI) across the adult years an into mid-life. BMI is a persons weight in kilograms divided by the square height in meters and serves as an easy screening method to determine if an individual is underweight, at an ideal weight, overweight, or obese. BMI has demonstrated a moderate correlation to body fatness (Flegal & Fraubard, 2009; According to the Centers for Disease Control and Prevention (2022), a healthy BMI is between 18.5 to 24.9. The CDC maintains an easy-to-use and interactive calculator which adults can use to determine whether they are within a healthy BMI range.
It is important to note that the overall pattern of body weight across the adult life span is usually in the form of an inverse or upside-down growth curve. Most persons will experience initial weight gain beginning in their 20’s and lasting until around the mid-50’s. By the time persons reach age 65 and older, they often experience unintentional weight loss. It is typically normal to lose one-quarter to a half pound of weight each year after turning age 65. Anything more should be considered abnormal and require consultation with a physician or dietician regarding a change in diet. Weight loss after age 65 is not due to a loss of fat. Rather, it is due to a loss of lean muscle, which is often attributed to a normative decreases in physical activity and movement that come with aging.
Sensory and Perception
Beyond the variety of bodily changes we might notice, two of the most commonly expected and normative age-associated changes in health include vision and hearing loss. There are no two ways around it. Most people will require some type corrective action to improve their vision and hearing by the time they reach middle age or enter into later life.
Vision
Around 50 years of age, most if not all persons will experience normal changes of the eye due to age is presbyopia, which is Latin for “old vision.” It refers to a loss of elasticity in the lens of the eye that makes it harder for the eye to focus on objects that are closer to the person. When we look at something far away, the lens flattens out; when looking at nearby objects tiny muscle fibers around the lens enable the eye to bend the lens. With age these muscles weaken and can no longer accommodate the lens to focus the light. Anyone over the age of 35 is at risk for developing presbyopia. According to the National Eye Institute (NEI) (2016), signs that someone may have presbyopia include:
- Hard time reading small print
- Having to hold reading material farther than arm’s distance
- Problems seeing objects that are close
- Headaches
- Eyestrain
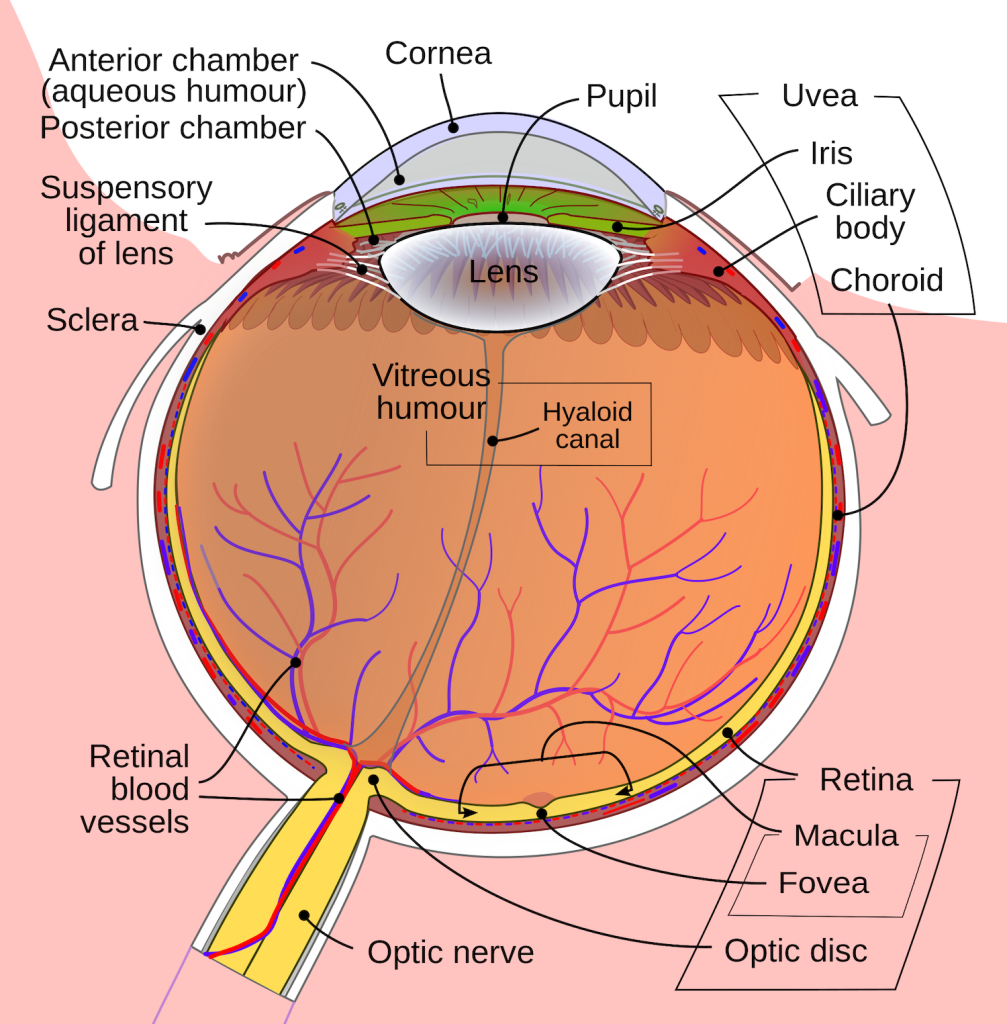
Loss of visual acuity is also normative age associated vision issue. The older we become the less likely we are able to make out the details of something seen at a distance. One vision problem that impacts how well an older adults can see are floaters, little spots or “cobwebs” that float around the field of vision. They are most noticeable if you are looking at the sky on a sunny day, or at a lighted blank screen. Floaters occur when the vitreous, a gel-like substance in the interior of the eye, slowly shrinks. As it shrinks, it becomes somewhat stringy, and these strands can cast tiny shadows on the retina. In most cases, floaters are harmless, more of an annoyance than a sign of eye problems. However, floaters that appear suddenly, or that darken and obscure vision can be a sign of more serious eye problems, such a retinal tearing, infection, or inflammation. People who are very nearsighted (myopic), have diabetes, or who have had cataract surgery are also more likely to have floaters (NEI, 2009).
During midlife, adults may begin to notice a drop visual acuity due to scotopic sensitivity, or the ability to see in dimmer light. By age 60, the retina receives only one third as much light as it did at age 20, making working in dimmer light more difficult (Jackson & Owsley, 2000). Night vision is also affected as the pupil loses some of its ability to open and close to accommodate drastic changes in light. Eyes become more sensitive to glare from headlights and street lights making it difficult to see people and cars, and movements outside of our direct line of sight (NIH, 2016c). Finally, some people experience dry eye syndrome, which occurs when the eye does not produce tears properly, or when the tears evaporate too quickly because they are not the correct consistency (NEI, 2013). While dry eye can affect people at any age, nearly 5 million Americans over the age of 50 experience dry eye. It affects women more than men, especially after menopause. Women who experienced an early menopause may be more likely to experience dry eye, which can cause surface damage to the eye.
Amid the experience of normative age-related changes in vision, it is estimated that 50% of adults over age 65 live with a visual disorder. The most common vision impairment or eye disease is a cataract, a clouding or opacity in the lens of the eye often reported as blurred or distorted vision, as well as a “yellowish” hue or tint. Some older adults even describe cataracts as seeing halos or similar to looking a pair of old tinted and blurry sunglasses. Cataracts begin developing in people around age 40 but do not impair vision until age 60 or older. By age 75, approximately half of all persons have cataracts. Cataracts start out as gradual visual cloudiness and progressively evolve into a more opaque visual field. They can impact quality-of-life in old age relative to experiencing difficulty reading, walking and maintain balance, watching television, recognizing faces, or engaging in work, hobbies, or leisure pursuits. Many older adult with cataracts also avoid driving during peak hours of sunlight, as well as at night. Thus, they become dependent on others for transportation. A variety of other age-associated conditions can further impact the onset and progression of cataracts, including obesity, high blood pressure, high blood sugar levels, and excess blood lipids (Poh et al., 2016). However, the use of sunglasses when outside, blue-light blocking lens when working in front of brightly lit screens, as well as a diet high in beta-carotene and vitamin C can keep the eyes health and protect against the severity of cataracts (Sideri et al., 2019). Luckily, cataracts can be easily treated through outpatient eye surgery. Persons who undergo surgical procedures to remove cataracts are usually in and out of an outpatient surgical center in an hour or less and return home to fully recover back to full vision within 7 days or less.

A second significant age-associated vision disorder includes age-related macular degeneration (ARMD), a visual condition caused by damage to the photoreceptors located in the central region of the retina or what is referred to as the macula. In other words, ARMD results in a blurred central field of vision. This retinal area is essential for being able to read, drive, and complete visually demanding and selective activities requiring use of one’s central vision. In ARMD, receptors in the macular are damaged the point that central vision is impaired and the individual must adapt by rely on peripheral vision fields. Nearly 9.1 million persons age 50 and older in the United have been diagnosed with late stage ARMD, a stage that can lead to severe vision loss and even permanent blindness. By the time persons reach 80 years of age, one in ten can expected to be diagnosed with ARMD. Women around the globe have been reported to be at greater risk than men for developing ARMD (Rudnicka et al., 2012; Sasaki et al, 2018).
There are two forms of ARMD. The “dry” form involves development of drusen in the macula, which are yellow deposits located under the retina. Drusen are easily detectable in persons aged 60 and older. The wet form entails the leaking of blood or fluid from the blood vessels in the retina. The wet form is most likely to rapidly progress and lead to a sudden loss of central vision. Roughly 10% of persons with ARMD are diagnosed with this wet type; thus most individuals are diagnosed as having the dry form of ARMD.
ARMD forms are clinically classified within clinically groups based on examination of the presence of drusen development in the macula (Ruia & Kaufman, 2023):
- Group 1: No ARMD/Sub clinical: No drusen or small drusen but no AMD pigmentary abnormalities; normal to impaired dark adaptations.
- Group 2: Early-stage ARMD: More than 15 small drusen or less than 20 medium-sized and indistinct soft drusen with pigment abnormalities without geographic atropy but dark adapatations.
- Group 3: Intermediate Stage: At least one large drusen or numerous medium sized drusen present, including those with indistinct as well as distinct boundaries; or presence of pigmentary abnormalities and impaired dark adaptations with non-central geographic atropy not involving the fovea.
- Group 4: Advanced Stage: Central geographic atrophy involving the fovea or presence of neovascular ARMD.
A final age-associated visual impairment is glaucoma, or a series of conditions involving the destruction of the neurons leading from the retina to the optic nerve due to increased pressure inside the eyeball. Glaucoma affects more than 2.7 million persons in the United States and represents the most common cause of blindness (NEI, 2016a). Persons over 40 years of age are most at-risk for developing this vision disorder. Over half of all persons diagnosed with glaucoma developed a common type that gradually develops undetected without any real symptoms. Thus, glaucoma can go undetected until the disease has reached advanced stages and it is too late to effectively treat with intervention. Glaucoma essentially involves loss of peripheral vision, and over time remaining vision may diminish altogether leading to complete blindness. In some cases, glaucoma symptoms arise suddenly and may include blurred vision, peripheral vision loss, perception of colored rings around lights, and pain or redness of the eyes. Interestingly, there are variations by sex, race, and health condition. For instance, glaucoma is more common among men than women, particularly those who are nearsighted. Furthermore, African-Americans over age 40 are 6-8 times more likely to be diagnosed with glaucoma than whites. Older adults with diabetes are also twice as likely to be diagnosed with glaucoma. There is no cure for glaucoma, but its rate of progression can be slowed, especially with early diagnosis. Routine eye exams to measure eye pressure and examination of the optic nerve can detect both the risk and presence of glaucoma (NEI, 2016b). Those with elevated eye pressure are given medicated eye drops. Reducing eye pressure lowers the risk of developing glaucoma or slow its progression in those who already have it.
Hearing
Almost 1 in 4 adults aged 65 to 74 and 1 in 2 aged 75 and older have disabling hearing loss (NIH, 2016). Table 9.4 lists some common signs of hearing loss. Presbycusis is a common form of hearing loss in late adulthood that results in a gradual loss of hearing, particulary high-pitched sounds. This has an effect on an older adult’s ability to engage in and understand normal conversation and can thereby cause an older adult to avoid noisy social situations or larger gatherings, such as eating in a restaurant or attend group meetings or celebrations (Murphy et al., 2006). Presbycusis is also believed to be hereditary within families and can affect the hearing or a single as well as both ears (NIA,2015c). The single best way to reduce and minimize the risk of hearing loss due to presbycusis is to reduce your exposure to noise. Older adults may also notice tinnitus, a ringing, hissing, or roaring sound in the ears. The exact cause of tinnitus is unknown, although it can be related to hypertension and allergies. It may also be potentially related to the use of aspirin, antibiotics, and anti-flammatory medications, past history of head trauma or concussion and the build-up of wax in the ears. It may come and go or persist and get worse over time (NIA, 2015c). The incidence of both presbycusis and tinnitus increase with age and males have higher rates of both around the world (McCormak, Edmondson-Jones, Somerset, & Hall, 2016). The auditory system has two jobs: To help hear, and to help maintain balance. Balance is controlled by the brain receiving information from the shifting of hair cells in the inner ear about the position and orientation of the body. With age this function of the inner ear declines which can lead to problems with balance when sitting, standing, or moving (Martin, 2014).
| Common Signs of Hearing Loss |
|---|
| Have trouble hearing over the telephone |
| Find it hard to follow conversations when two or more people are talking |
| Often ask people to repeat what they are saying |
| Need to turn up the TV volume so loud that others complain |
| Have a problem hearing because of background noise |
| Think that others seem to mumble |
| Cannot understand when women and children are speaking |
Balance
Sense of balance becomes increasingly important with age. It can be the different between unintentional injury and hospital admission, as well as life and death. In fact, poor balance is one of the main factors associated with falls in older adults. Falls are preventable, yet one out of every four older adult, aged 65 and older fall each year in the United States. This equates into over 36 million falls involving older adults reported yearly, resulting in more than 32,000 deaths. Another 3 million older adults treated annually in hospital emergency room departments for an unintentional fall injury. Of those who fall, nearly 75% are women who have fractured their hip, usually due to falling sideways. Thus, age-associated changes in balance should be taken seriously.
It is natural for persons who have had a painful and frightening fall in the past to remain feeling anxious and insecure about any future subsequent or similar fall. The fear of falling can be a vicious cycle in which older adults increasingly restrict their movement and avoid any situations which might make them feel uneasy about ambulating across time and environmental space. In a sense, fear of falling can be adopted by older adults as part of their identity, and thus they can lose confidence in their ability to walk or avoid a fall and eventually encounter other negative physiological outcomes (Horslen et al., 2015). Interestingly, researchers have reported mixed results relative to whether being infected with COVID-19 or obeying stay-at home restrictions increased falls risk or fear of falling among older adults during or after the pandemic (Gawronska & Lorkowski, 2021; Kiyoshi-Teo et al., 2022; McIntyre, Prichett, & McNabney, 2022).
Nonetheless, there are two conditions associated with age-related vestibular dysfunction. These include dizziness and vertigo. Dizziness is an uncomfortable sensation of feeling light-headed and unbalanced. Vertigo refers to the sensation of that one is spinning despite being stationary or at-rest. The vestibular system is so intricately interconnected to other parts of the nervous system that persons may experience a variety of symptoms such as headaches, muscular aches in the neck and back, or increased sensitivity to noise or bright lights. In addition, some persons may report feeling fatigued, unable to concentrate, unsteady while standing, or unable to formulate words. Some of these changes are due to other conditions or diseases of normal aging; whereas others occur as a result of normal alterations in vestibular receptors. Recent evidence on the origins of vertigo suggest that over 50% of vertigo cases in older adults can be traced to three predominant origins (Fancello et al., 2023) approximated as 28.4% attributed to audio-vestibular disorders (conductive and sensorineural hearing loss), 20.4% due to cardiovascular conditions (e.g., hypertension, arrhythmia, ischemic heart disease), and 15.1% connected to on-going neurological diseases (e.g., migraine headache, cerebrovascular disorder, traumatic head injury).
Although older adults may be impacted by dizziness and vertigo, risk of falling is preventable. From a basic practical level, the older adults should sit upright or lie down immediately while tilting their head away from the side in which they feel the sensation of dizziness or vertigo the most. Furthermore, the older adult should avoid drinking caffeine and instead opt to drink more water in order to stay hydrated. Exercise can also help reduce the chances of dizziness and vertigo as well as compensate for factors that might otherwise increase the risk for following. Such exercises include practice relative to maintain proper posture and balance. Other recommended solutions might include having one’s ears checked by an audiologist for wax build-up or other inner ear infection or issue, visiting the eye doctor in order to check that one’s vision or eyeglasses do not need correction, providing adaptative devices such as grab bars within the home, walking sticks or canes, improved hallway lighting, or providing a bench or stool which can be used to sit while cooking or even taking a shower.
Taste and Smell
Have you ever heard an older loved complain about the taste of food, request for the salt and pepper, and proceed to over-season their food? Better yet, have you ever observed an older adult who seems to have a sweet tooth and enjoys eating abundance of chocolate or other types of candies? The reason for such behaviors may stem from normative age-related changes in taste and smell. The sense of taste and smell are part of our chemical sensing system. Our sense of taste, or gustation, appears to age well. Normal taste occurs when molecules that are released by chewing food stimulate taste buds along the tongue, the roof of the mouth, and in the lining of the throat. These cells send messages to the brain, where specific tastes are identified. After age 50 we start to lose some of these sensory cells. Most people do not notice any changes in taste until ones 60s (NIH: Senior Health, 2016b). Given that the loss of taste buds is very gradual, even in late adulthood, many people are often surprised that their loss of taste is most likely the result of a loss of smell. Our sense of smell, or olfaction, decreases more with age, and problems with the sense of smell are more common in men than in women. Almost 1 in 4 males in their 60s have a disorder with the sense of smell, while only 1 in 10 women do (NIH: Senior Health, 2016b). This loss of smell due to aging is called presbyosmia. Olfactory cells are located in a small area high in the nasal cavity. These cells are stimulated by two pathways; when we inhale through the nose, or via the connection between the nose and the throat when we chew and digest food. It is a problem with this second pathway that explains why some foods such as chocolate or coffee seem tasteless when we have a head cold. There are several types of loss of smell. Total loss of smell, or anosmia, is extremely rare.
Problems with our chemical senses can be linked to other serious medical conditions such as Parkinson’s, Alzheimer’s, or multiple sclerosis (NIH: Senior Health, 2016a). In fact, some clinicians use a diagnostic test for dementia referred to as the peanut butter test, in which they measure an older patient’s ability to detect and smell peanut butter through each nostril (Stamps et al., 2013).
If any sudden changes in a older adult’s ability to taste or smell does occur, then it should be checked out. Loss of smell can change a person’s diet, with either a loss of enjoyment of food and eating too little for balanced nutrition or adding sugar and salt to foods that are becoming blander to the palette. Such dietary changes can lead to complications relative to high blood pressure, spikes in blood glucose levels, and malnourishment.
| Types of Smell Disorders | |
|---|---|
| Presbyosmia | Smell loss due to aging |
| Hyposmia | Loss of only certain odors |
| Anosmia | Total loss of smell |
| Dysosmia | Change in the perception of odors. Familiar odors are distorted. |
| Phantosmia | Smell odors that are not present. |
Touch
With advancing older age, people may experience reduced or changed sensations of vibration, cold, heat, pressure, or pain (Martin, 2014). Many of these changes are also aligned with a number of medical conditions that are more common among the elderly, such as diabetes. However, there are changes in the touch sensations among healthy older adults. The ability to detect changes in pressure have been shown to decline with age, with it being more pronounced by time persons reach age 60 and older (Bowden & McNelty, 2013). Yet, there is considerable variability, with almost 40% showing sensitivity comparable to younger adults (Thornbury & Mistretta, 1981). However, the ability to detect the roughness/smoothness or hardness/softness of an object shows no appreciable change with age (Bowden & McNulty, 2013). Those who show increasing insensitivity to pressure, temperature, or pain are at greater risk for potential injury (Martin, 2014).
Pain
According to Molton and Terrill (2014), approximately 60%-75% of people over the age of 65 report at least some chronic pain, and this rate is even higher for those individuals living in nursing homes. Although the presence of pain increases with age, older adults are less sensitive to pain than younger adults (Harkins, Price, & Martinelli, 1986). There is a lack of evidence to suggest that older adults become immune from the sensation of pain by the very fact of experiencing a multitude of age-associated sensory changes. Farrell (2012) looked at research studies that included neuroimaging techniques involving older people who were healthy and those who experienced a painful disorder. Results indicated that there were age-related decreases in brain volume in those structures involved in pain. Especially noteworthy were changes in the prefrontal cortex, brainstem, and hippocampus. Women are more likely to identify feeling pain than men (Tsang et al., 2008). Women have fewer opioid receptors in the brain, and women also receive less relief from opiate drugs (Garrett, 2015).
Because pain serves an important indicator that there is something wrong, a decreased sensitivity to pain in older adults is a concern because it can conceal illnesses or injuries requiring medical attention. Chronic health problems, including arthritis, cancer, diabetes, joint pain, sciatica, and shingles are responsible for most of the pain felt by older adults (Molton & Terrill, 2014). Cancer is a special concern, especially “breakthrough pain” which is a severe pain that comes on quickly while a patient is already medicated with a long-acting painkiller. It can be very upsetting, and after one attack many people worry it will happen again. Some older individuals worry about developing an addiction to pain medication, but if medicine is taken exactly as prescribed, addiction should not be a concern (NIH, 2015b). Lastly, side effects from pain medicine including constipation, dry mouth, and drowsiness may occur that can adversely affect the elder’s life.
Some older individuals put off going to the doctor because they think pain is just part of aging and nothing can help. Of course, this is not true. Managing pain is crucial to ensure feelings of well-being for the older adult. When chronic pain is not managed, the individual will restrict their movements for fear of feeling pain or injuring themselves further. This lack of activity will result in more restriction, further decreased participation, and greater disability (Jensen, Moore, Bockow, Ehde, & Engel, 2011). A decline in physical activity because of pain is also associated with weight gain and obesity in adults (Strine, Hootman, Chapman, Okoro, & Balluz, 2005). Therefore, managing or controlling one’s weight would most likely be a one effective intervention to enhance quality of life across the life-span. Additionally, sleep and mood disorders, such as depression, can also occur (Moton & Terrill, 2014). Learning to cope effectively with pain is an important consideration in late adulthood and working with one’s primary physician or a pain specialist is recommended (NIH, 2015b).
Vital Bodily Functions
Aging and Muso-Skeletal System Functioning
Mobility is essential to human health and aging. It is considered one of the underlying secrets to living a long life. Our ability to move around and about in our environment is a vital source of autonomy in everyday functioning. Our bones, muscles, tendons, and ligaments are interconnected structures that allow humans to move. On average, each of these structures undergo significant observable change once persons cross the threshold of 40 years of age. Around this time, persons are likely to notice significant age-related losses in walking speed that require them to more intentionally adapt how they move within various spaces over time without making a catastrophic mistake that could lead to an unintentional fall of injury (Dommes et al, 2012). It’s a simple fact of aging. Humans walk slower with age (Asher et al., 2015; Dommes et al., 2012; Shumway-Cook et al., 2007). Even a simple task, such as crossing the street, takes us more time to do the longer we live and the older we become (Asher et al., 2015; Dommes et al. 2012). Decline in mobility has been linked to normative age-associated changes in the gait cycle, or the sequential action of walking (Jerome et al., 2015). A gait cycle consists of two primary phases:
- Stance phase or act of walking in which some part of the foot is in contact with the ground and
- Swing phase or act of walking in which the foot is not in contact with the ground and one’s bodyweight is borne by the other leg or foot.
Normative age-related changes come in the form of slower movement, impaired coordination, balance and stability, reduced muscle strength for weightbearing support in the lower extremities, and increased risk of falling. There is no doubt that many of these age-associated changes are influenced by various foot problems, such as bunions, fungal infections, heel spurs, poor circulation, and nerve damage. In fact, it is very common for older adults to experience neuropathic pain or neuropathy in the feet (Giovannini et al., 2021). Neuropathy entails peripheral nerve damage usually located in the hands or feet which causes sensations such as numbness, tingling, burning, and sharp and stabbing pain. Neuropathy commonly occurs in the presence of other morbidities, such as diabetes, vitamin deficiencies, inflammation, autoimmune disorders, or as a side-effect from taking various toxic medications commonly used in chemotherapy cancer treatments (Bouche, 2020). Approximately 5-7% of all adults over the age of 45 suffer from neuropathy. However, an estimated 50% of all older adults, aged 65 and older, diagnosed with diabetes report symptoms of neuropathy impacting their lower extremities during their lifetime (Hicks & Selvin, 2019). It is further estimated that nearly 10 to 20% of all older adults suffer from some form of neuropathic pain that negatively impacts their ability to walk or ambulate, yet they remain clinically undiagnosed (Bouche, 2020; Giovannini et al., 2021).
Muscles
Our adult years are also characterized by age-associated loss of muscle mass. Consequently, we lose strength and become physically weaker as we age. This has a lot to do with a process known sarcopenia, a geriatric disease characterized by the progressive loss of skeletal muscle mass and decrease in the size and number of fast-twitch muscle fibers responsible for our physical speed and strength (Rosenberg, 1997). When sarcopenia reaches severe levels, it sometimes referred to “muscle wasting.” This is commonly seen in older adults who have spent an extended duration of time bed bound, such as in a hospital or care facility, with little to no physical movement, exercise, or weight and resistance training. Interestingly, muscle strength peaks in our 20’s and 30’s, plateaus in our 40-50’s, and declines at a rate 12-15% faster per decade after reaching 60 (Kostka, 2005). Diminished muscle strength tends to be more pronounced among men. By the time persons reach their 80’s, approximately 50% of all muscle fibers have been lost (Faulkner et al, 2007). Changes in muscle mass are highly associated with age-related decline in strength during our middle and older adult years (Walston, 2012). Loss in muscle strength also occurs from disruption and misfiring of neurotransmission signals within the nervous system that make the muscles contract (Clark & Fiedling, 2012). Finally, the tendons of our joints become more rigid with age. Thus, it becomes difficult and requires greater exertion of muscular strength to create movement in individual joints of the body (Carroll et al., 2008).
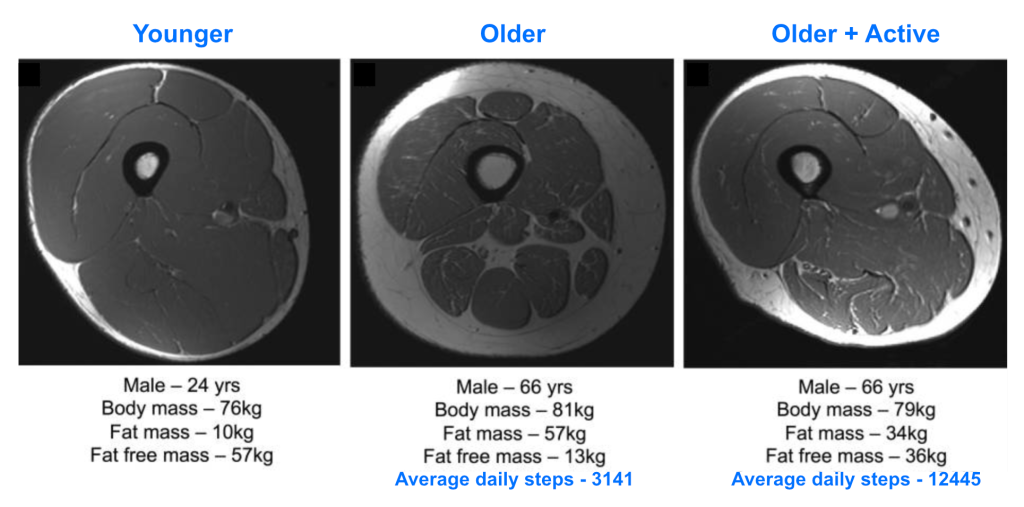
As persons age, they normatively engage in lower levels of physical activity. This is one primary contributing risk factor of sarcopenia. Muscle mass decline is further complicated by normative dietary changes that come with aging, such as a decreased appetite or meal-skipping which leads to reduced intake of nutrient and caloric rich foods high in vitamin D and protein (Papadopoulou, 2020). In fact, older adults generally consume 25% less food than they did when younger (Alexandre et al., 2014). Other contributing age-associated risk factors of sarcopenia include genetics, low birth weight, diminished testosterone and estrogen in men and women, chronic inflammation, and poor sleep quality (Papadopoulou, 2020).
Loss of muscle mass put older adults at-risk for falling, limiting mobility, and reduced quality-of-life. Sarcopenia can severely compromises engagement in activities that older adults might enjoy the most. For example the greater the loss in muscle mass; the more difficult it can be to participate in a daily exercise routine, which only leads to more weakening of the muscles (Lang et al., 2009; Papadopoulou, 2020). There is also the possibility that older adults might experience a condition known as, sarcopenic obesity, or muscle loss in the presence of gains in overall body fat.
One of the most effective preventions against sarcopenia is strength training whether with free weight or resistance exercises (Nascimento et al. 2019; Papadopoulou, 2020). Every little bit counts when it comes to resistance-based strength training programs. This is evidence by the fact that older adults show improvement relative to gaining fast-twitch muscle fibers both in number and size in just under 16 weeks of engaging in resistance training (Negaresh et al., 2019). Age is not a good excuse for preferring not to exercise and strengthen one’s muscles. Older adults well into their 90’s have been reported to demonstrate gains in overall muscle strength. The stronger we can keep our muscles, the better we will be relative to being able exert the force necessary to walk, push, and pull.
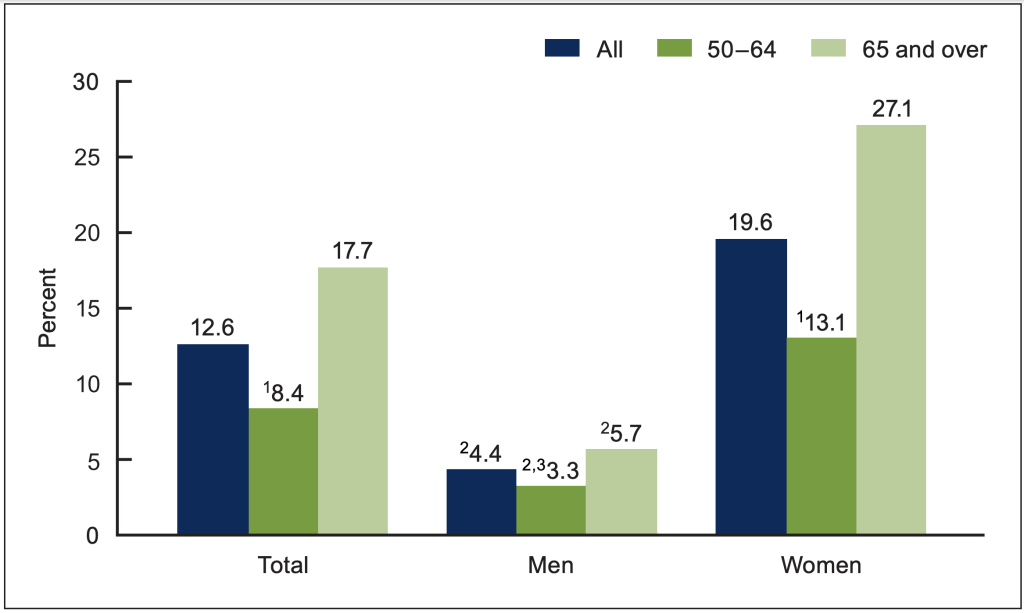
Bones
Bone is a composite structure and genetically living tissue, consisting of cells, lipids, minerals and water (Boskey & Coleman, 2010). There is a prevailing misconception that our bones are rather static, never-changing, and likened to a skeleton that sits in the closet of an anatomy classroom only to be brought out whenever the instructor is addressing the topic of bone identification. The opposite is true. Our bones are constantly changing as we age. Bone is constantly reconstructing and repairing itself through a process called bone remodeling, which involves a set of protein-like substances that act on bone cells, whereby old cells are destroyed and replaced by newly regenerated cells. These substances are under the direction of sex hormones, estrogen for women and testosterone for men. As a result, as person age and experience decrease sex hormone production, and they also lose bone mineral content (Sigurdsson et al., 2006). Consequently, this contributes more brittle and weaker bones at older ages. However, there are reported sex and racial differences. For example, bone mineral content has been estimated to decrease about 0.5% for men and 1% per year for women (Emaus et al., 2006). These rates increase and range from 3-5% for women as they reach 50-years of age, with white post-menopausal women showing higher rates of bone loss than black post-menopausal women; whereas the reverse is true among men (Conradie et al., 2015; Sheu et al., 2009).
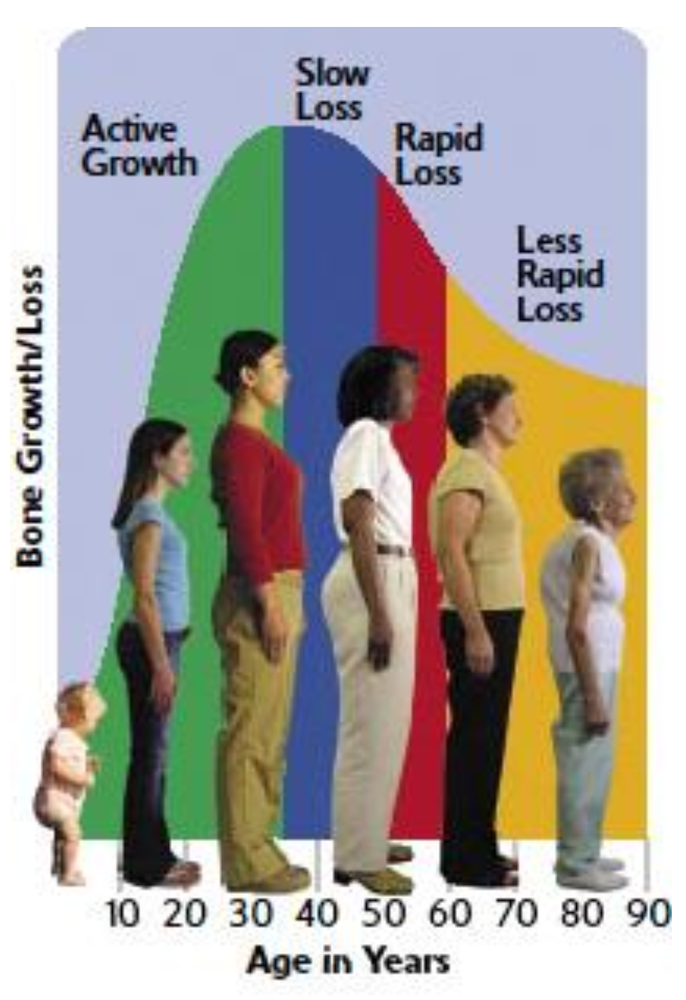
Additional weakening of the bones occurs due to microcracks. The older we become the more brittle and fragile our bones become. This should come as no surprise. Bone is continuously and repetitively loaded and under stress during the normal activities of daily life, as well as extreme periods of exercise and conditioning throughout the course of life. In turn, our bone naturally develops cracks over time, initially invisible at the sub-micron level, but these cracks become visible with aging, especially if not repaired during the bone remodeling process (O’Brien et al., 2005). A part of that aging bones risk of fracture can be explained by a loss of collagen, which reduces bone flexibility in response to pressure (Saito & Maumo, 2009). The extent of this micro-damage leading to failure or fracture increases exponentially with age (Schaffler et al., 1995). This can be particularly detrimental for the upper part of the thigh bone just beneath the hip, which has limited mechanical pressure and tends to disproportionately thin with normative aging. In studies investigating old-old adults, persons age 85 and older, the incidence of bone fracture has been reported to be 10-15 times more likely than for persons aged 60-65 (Tommasini et al., 2007;Melton, 1996; Yates et al., 2007). Hip fractures can be especially lethal for older adults. Continued survival for old men and women following a hip fracture is significantly reduced. The absolute mortality risk one-year after a hip fracture has been reported to be 21.5% in women and 32.3% in men (Brown et al., 2021)
Our bones remain healthy into old and very old age only to the extent that engage in positive lifestyle choices and behaviors. Persons who elect to live a sedentary life, smoke and drink, eat protein deficient foods, and have inadequate in-take of calcium and Vitamin D showing accelerated rates and greater prevalence of bone loss in later life (Shapse & Sukumar, 2012). Conversely, individuals who engage in daily or routine exercise (both aerobic and resistance), maintain a balanced diet rich in nutrients, do not smoke and resist the temptation to binge drink or consume large amounts of alcohol, and maintain adequate in-take of calcium and Vitamin D are likely to delay the rate and prevalence of bone loss into advanced older ages.
Interestingly, bone health may also depend on where persons reside. Mounting evidence suggests that environment shapes bone health over time. Persons who live in regions where climates have sharp demarcations between seasons, including but not limited to longer periods of cloud cover and reduced duration of sun exposure, are more likely to be diagnosed with early onset bone loss. For instance, persons living in Norway have some of highest rates of bone loss than anywhere else in the world (Formso et al., 2005); whereas persons living in India have lower prevalence of bone loss or risk of fracture (Shen et al., 2022). Such differences are associated with exposure to sunlight and Vitamin D production, which greatly benefits bone health for older adults.
Joints
Joint pain is one of the more common complaints of aging. Unlike our muscles, joints benefit little from continuous and repeated daily use. Rather, the opposite is true. Joints are effectively damaged with overuse. At some point during our lifetime, many have probably played a sport, participated in an exercise class, hiked, jogged, or even participated some other physically demanding activity. By the time we reach our 20’s and 30’s, the articular cartilage that protects the joints has already begun to deteriorate and the fibers within the joint capsule become less flexible, which also had negative consequences for our bone health. This normative aging process impacts our knees, limbs, hands, ankles, and feet and persons find it increasingly harder to move, walk, sit down and stand up, or even roll in and out of bed. Joint pain especially impacts mobility and quality-of-life among middle aged women as early as 40 years of age (Ding et al., 2017). Individuals should take precautions during the emerging adult year to reduce the risk developing joint stiffness or pain. Some sound advice includes eating a balanced anti-inflammatory diet consisting of a lot of fruits and vegetables, managing one’s weight within a healthy BMI range, wearing supportive foot wear during high-impact exercise or sport participation, making swimming or water aerobics a part of your exercise routine, and engaging in daily stretching exercises to maintain flexibility.
Aging and Cardiovascular Functioning
Our major bodily organs are the source of life. Remaining aware of age-associated changes impacting the heart, lungs, kidney, and stomach is essential to avoiding acute and chronic diseases and remaining active and healthy in old age. This requires understanding of each system, as well as knowledge regarding how to modify our behavior in terms of managing psychological and socio-emotional stressors, eating a balanced diet, and staying physically fit.
Heart health is vital to human survival. The heart is part of the cardiovascular system which also consists of the arteries circulate oxygenated blood throughout the body and away from the heart, as well as veins which carry blood back to the heart for oxygenation. The heart muscle itself and supporting arteries go through some of the most significant age-associated changes unlike other major organs of the body; whereas our veins are left mostly intact.
To review the structural and mechanical operation of the heart, there are two ventricles: (1) the left ventricle is the chamber responsible for pumping oxygenated blood out to the arteries throughout the body and; (2) the right ventricle right ventricle pumps oxygen-poor blood from out veins to the lungs for elimination of CO2 and oxygenation. Cardiovascular efficiency is evaluated by aerobic capacity, or maximum amount of oxygen that can be delivered through the blood; and cardiac output, the amount of blood that heart pumps per minute. From age 20 to 70 years of age, aerobic capacity will decline on average by 5-10% per decade. Around age 30 to 40 years this decline amounts to 3-6% per decade, and by age 70 the rate increases to approximately 20% per decade. Thus, physical activity as well as exercise are vital to staying fit and managing heart health despite normative loss in functioning.
Arteries are further regulated by lipid metabolism. High-density lipoproteins (HDLs) or good cholesterol help transport lipids out of the body; whereas Low-density lipoproteins (LDLs) or “bad” cholesterol deliver cholesterol to the arteries. Cholesterol is an essential marker of overall cardiovascular wellness and thus cholesterol biomarker levels are commonly evaluated as the ratio of HDLs and LDLs. In addition, blood levels of triglycerides are another biomarker use to reflect the total amount of fat that is being stored in the body’s cells. Moderate levels of exercise help manage cholesterol levels, yet persons who remain sedentary and smoke across their lifetime tend to have higher inflammatory biomarker levels in their blood (Yilmer & Kayancicek, 2018).
Many of the health-related problems older people experience with their heart and blood vessels are caused by disease and not by aging. For example, an older heart can normally pump blood as strong as a younger heart, while less ability to pump blood is caused by disease. Therefore, leading a heart-healthy lifestyle is most important to keeping one’s heart strong through mid-life into late adulthood.
Aging and Respiratory Functioning
Normal aging impacts all functions of our respiratory system. Our respiratory systems helps bring oxygen into the body, as well as remove carbon dioxide. The is accomplished through breathing, a mechanical process involving contraction of the diaphragm and muscles of chest wall, which exchange gases. This process takes place within the alveoli, tiny air sacs located within the airways of the lungs. The lungs are fully developed by the time person reach 20-25 years of age (Sharma & Colemant, 2006). However, the respiratory muscles become less effective in promoting the expansion and contraction of the chest wall, and lung tissue itself is also unable to fully expand and contract during inhalation. By the time humans reach 40 years of age, all measurable indicators of lung functioning begin to show age-related declines. The result of such losses involve difficulty breathing whenever the body is under physical duress. According to the American Lung Association (2023), the most common age-associated respiratory changes include:
- Alveoli losing their shape
- Weakening of the diaphragm
- Alteration and thinning of the ribcage bones making is more difficult to expand and contract when breathing;
- Nerves in the airway that trigger coughing become less sensitive to particle;
- Reduced immunity increases risk of contracting the flu and pneumonia
To protect the lungs from normative age-related changes it is highly recommended that older persons avoid smoking, minimize exposure to air pollution, engage in daily aerobic exercise, practice weight management, and frequently stand up and move rather than lay down while awake during the day.
Aging and Urinary System Functioning
The kidneys, bladder, ureters, and urethra comprise the urinary system. The main function of this system is to excrete and remove waste from the baby in the form of urine The kidneys are made up of nephrons, cells that operate of as tiny filters to cleanse and rid the body of metabolic waste. These waste products combing with excess water from the blood and are eliminated through the urethra.
The kidneys undergo several age-related changes. Renal aging involves a complex array of genetics, environment, and cellular processes that lead to structure and functional changes in the kidneys. Structural age-changes in the kidneys can be divided into two broad categories: (1) micro-anatomical and; (2) macro-anatomical (Denic et al., 2016). On a micro-level, there is a decline in the total nephron size leading to a reduced rate at which waste is filtered and removed from the body (O’Sullivan et al., 2017). This believed to be initiated by atereriosclerosis of the small arteries in the kidney which cause an ishemic injury to the nephrons. This can lead to nephrosclerosis or irreversible chronic changes in kidney functioning. Normative aging also brings about macro-level changes in blood flow through the kidneys and an increased inability to raise and lower the volume concentration or urine starting around age 50 and has a greater impact on women than for men (Karam & Tuazon, 2013; Denic et al., 2016). An additional common macro-level change with older age includes the greater risk of developing benign kidney cysts, round pouches of fluid that form on the surfaces of the kidneys and impair the flow of urine. Kidney cysts that burst can cause fever and severe back pain, as well as produce blood in the urine. Health care professionals must be aware of several other counteraction processes that impact kidney health when dealing with older adults, namely stress placed on the kidneys due to infection or illness, physical exertion, or exposure ot extreme heat (Esposito et al., 2007). Thus, when trying to prescribe medications or interventions to treat kidney issue in geriatric patients, prescription dosages used to treat other health problems, such as antianxiety medications, anticoagulants, and antibiotics symptoms, must be accounted in order not to further harm kidney functioning (Guerville et al., 2019).
The bladder also undergoes extensive change as persons age. A common problem for most older adults is no longer being able to effectively and efficiently retain or expel urine. The bladder does not shrink with age, however the perception of when and if one has to urinate certainly does change with advanced age. For instance, many aging men experience hypertrophy or enlargement of the prostate gland, which is anatomically located on top of the bladder. This puts pressure on the bladder and can lead a sudden perception and urge to urinate without much warning, or what is termed urge incontinence. In some cases, accidental leakage of urine can happen. Approximately 35% of community-dwelling adults in the United States over the age of 60 suffer from urinary incontinence, whereas this proportion increases to more than 50% among older adult residents in long-term care setting (McDaniel et al., 2020. Milsom & Gyhagen, 2018). Urge incontinence is closely related to overactive bladder, or the feeling that one needs to urinate which can occur more frequently than normal or even immediately following urination in the absence of infection, kidney stones, or other pathology (Suskind, 2017). Overactive bladder is estimated to effect nearly 40% of older men and 30% of women after the age of 75 (Milsom et al., 2000). Many times, overactive bladders goes untreated. In fact, it is estimated that nearly 76% of older adults with diagnosable symptoms for overactive bladder are untreated (Hefland et al., 2009). Finally, older adults can also experience stress incontinence, whereby the individual is unable to retain urine while engaging in some form of physical exertion, such as a sneezing, coughing, or exercising.
There is a clear gender disparity when it comes to problems with incontinence. As a whole, older women are five times more likely to experience daily urinary incontinence compared to older men. Despite the fact that many men may be challenged by enlarged prostates, older women generally experience more progressive degenerative changes relative to pelvic muscle fibers, reduced bladder capacity, and abnormal or low control over bladder contraction (Wilson, 2003). Reasons for this gender difference vary, however it is believed that lifetime experiences including childbirth, need for gynecological procedures, and hormonal changes that accompany menopause are likely contributory variables (Wilson 2003). However, there are treatment alternatives for incontinence and overactive bladder ranging from behavioral monitoring of dietary fluid intake and tracking bathroom visits, to pelvic floor or “Kegel” exercises involving strengthening the urinary sphincters through contraction and relaxation (Felicissimo et al., 2010)
Aging and Digestive System Functioning
Our digestive system is also impacted by normative aging. The digestion of food begins with the breakdown of nutrients in food via the secretion of saliva from the salivary glands. However, salvia production decreases with age (Elliason et al., 2006). This results in a less than efficient ability to process certain foods. Oral health changes including but not limited to reduced mobility of the lower jaw, gum disease, tooth decay and loss, and use of dentures can make it more difficult to eat certain foods that may be hard in texture. Furthermore, changes in the esophagus involving reduced effectiveness in contracting and expanding to help move food down into the stomach also impact the digestive process in later life (Cook & Omari, 2018). Finally, the stomach secrets fewer gastric juices with age. This is a necessary process of digestion which results in a reduced rate in the breakdown of food and expulsion from the body as solid waste (Remond et al., 2015). In turn, age-associated gastrointestinal changes can contribute to a number of other complications including but not limited to malnourishment, stomach ulcer, fecal incontinence, or constipation.
Fecal incontinence increases with age and involves the accidental leakage or passing of bowel movements in the digestive process. An estimated 7-15% of able-bodied adults have fecal incontinence (Whitehead et al., 2016); whereas between 50-70% of older adults residing and receiving long-term care have been reported as challenged by accidental bowel movements. When it does occur, fecal incontinence is very embarrassing for the older adults. As true with urinary incontinence, preventative behavioral training to ward off the sudden urge to defecate can help older adults regain control over a common bodily function and even improve their sense of autonomy and control in life (Olsson & Berero, 2014). In addition, increasing daily consumption of foods high dietary fiber, such as beans and lentils, whole grains, vegetables, and dried fruits, is also a common solution.
Meanwhile, one of the most common digestive complaints among persons beginning around age 50 and continuing into later adulthood is constipation. Constipation is a condition in one the person has fewer than three bowel movements in a given week and in which stools are hard, dry, lumpy, and often difficult and painful to pass. According to the Rome III Criteria for Adults used to diagnose constipation, an older adult is considered to have constipation when at least two of the following symptoms have occurred in the previous 3 months with an onset of symptoms of at least 6 months including:
- Straining to pass fecal matter or stool
- Hard and lumpy stool
- A sense of incomplete evacuation of stool
- A sense of anorectal obstruction
- Need for manual maneuvers
- Fewer than 3 defecations per week
- Loose stools rarely present without use of a laxative
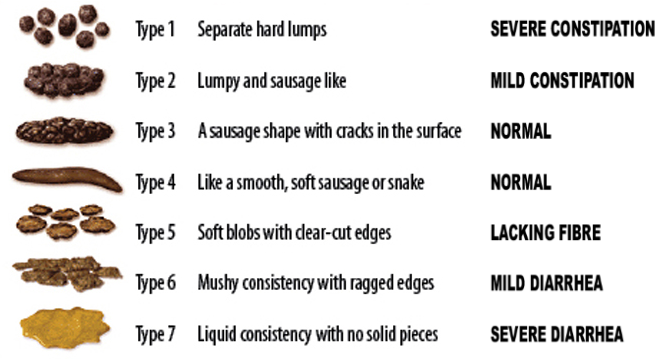
Among individuals 65 years of age and older, 26% of women and 16% of men are clinically reported as having difficulty with constipation. By the time persons reach 85 years of age, this prevalence rate increases to 34% for women and 26% for men. Among older adults residing in long-term care settings, the prevalence rate can reach as high as 80% (Schuster et al., 2015). There are a multitude of known conditions believed to cause constipation among older men and women including normative age-associated hormonal changes, muscular atrophies or muscle wasting, eating disorders, kidney disease, diabetes, and feeling anxious or depressed. Older adults can also experience numerous side-effects from constipation including fever, bloody stool, unintentional weight loss, and severe abdominal pain. In some cases, chronic constipation can be symptomatic of a more serious underlying health issue requiring direct medical intervention such as dehydration, anemia or iron deficiency, colon cancer, or even neurological linked to Parkinson’s Disease and dementia (Schuster et al., 2015). The Bristol stool scale was developed by the Bristol Royal Infirmary (1997) as a diagnostic tool by which researchers, physicians, nurses, and family caregivers can evaluate various bowel problems, including constipation, whereby Type 1 and Type 2 of the scale indicate constipation.
Aging and Endocrine System Functioning
The endocrine system is complex and diverse set glands which control “target” organs via hormone production. Meanwhile, hormones are produced within the endocrine system serve as chemical messengers which regulate and control organ activity. With advanced age, changes occur relative to the regulatory pathways. A change in one pathway can create a chain-reaction in others whether it be a decrease or increase in the release of a particular hormone. Adding to the complexity of this process is the fact that the endocrine system can be particularly sensitive to acute and chronic illness as well as exposure to physiological stress. One vital gland includes the pituitary gland, located deep within the base of the brain and controlled by hypothalamus and anterior (front) section of this gland. Hypothalamus-releasing factors (HRFs) are produced in the hypothalamus which in turn help to regulate secretion of hormones produced by the anterior pituitary gland. It is important to note that the hypothalamus is a structure also part of the nervous system, thus it is considered a neuroendocrine structure, to the extent that it may release HRFs in response to information sent from various parts of the nervous system.
Six key hormones linked to the aging process are produced within the anterior pituitary gland including:
- Growth Hormone (GH; referred to as somatotropin)
- Adrenocortiotrophic hormone (ACTH)
- Thyroid stimulating hormone (TSH)
- Follicle stimulating hormone
- Leutenzing Hormone (LH)
- Prolactin
Growth Hormone
Throughout infancy through adolescence, growth hormone (GH) stimulates the growth of our bones and muscles and regulates the growth of our internal organs. Physiologically, GH is responsible for directing the metabolism of proteins, lipids, and carbohydrates within normal food intake. A closely related hormone produced in the liver, insulin-like growth factor-1 (IGF-1) stimulates the number and mass of muscle cells. GH and IGF-1 work together but with advanced aging there is a decline in their activity. This process is referred to s somatopause of aging, which is associated with age-related changes in body composition including loss of bone mineral content, increase fat, reduced muscle mass, and loss in physical strength and endurance through the adult years (Lombardi et al., 2005). When we are younger, GH rises during periods of physical exercise but in persons age 60 and older it is generally diminished.
GH plays an important role within so many basic biological processes of aging. In face some aging experts and even older former professional athletes and modern-day celebrities, such as Mike Tyson, Suzanne Somers, and Sylvester Stallone, have advocated GH replacement therapy as an antidote to counter the signs, symptoms, and effects of age-associated health declines. It does appear that GH replacement therapy helps reduce fatty mass and enhance lean muscle, but there is a lack of overall evidence that it can increase muscle strength, enhance physical and athletic performance, or improve quality-of-life. Thus, despite the fact that many older former athletes and celebrities suggest GH replacement therapy can reverse aging, there is sufficient longitudinal evidence to justify continued administration and use in persons over age 65 (Samaras et al., 2016). Instead, there is increasing evidence that long-term GH replacement therapy may actually increase negative side-effects for some persons in terms of cardiovascular morbidities (Tidbland et al., 2021).
Cortisol
Cortisol is a hormone produced by the adrenal gland. Cortisol has been used a key biomarker within the saliva and blood as an indicator of physiological stress. Cortisol actually functions to energize the body, particularly in fight and flight situations, where the body may require energy to the muscles to prepare them for reaction and action. Therefore, cortisol is commonly referred to as a “stress hormone” within many physiology of aging studies. The perspective that aging causes dangerous spikes in cortisol levels is referred to as the glucocorticoid cascade hypothesis (Angelucci, 2000). This hypothesis suggests that increased cortisol level accelerates neuronal losses in the hippocampus of the brain, which is a key center for memory. A high activated cortisol level or an elongated sustained time period can be symptomatic of future poor cognitive functioning in the form of memory deficient including memory complaint, forgetfulness, and permanent loss (Comijs et al., 2010), yet more recent research has called such associations into question providing evidence that contextual conditions under which environmental stressors originate and operate may provide a more plausible explanation of how cortisol levels impact aging our body and mind (Sindi et al., 2014).
Thyroid Hormones
The thyroid is a small butterfly-shaped gland in the front of the neck that produces hormones which control basal metabolic rate (BMR) or what is otherwise metabolism. BMR shows signs of slowing around middle age, as evidenced by increased weight gain, fatigue, mood disturbances despite caloric in-take and activity levels remaining the same. There are three types of hypothyroidism (See Figure 4.8):
- Primary (under-stimulation of the thyroid gland in which there are low levels of thyroid hormones being produced;
- Secondary (pituitary gland fails to stimulate thyroid to produce enough thyroid hormones)
- Tertiary (inadequate secretion of hormones from malfunctioning of the hypothalamus leads to insufficient thyroid stimulation)
Hashimoto’s Diseases is most common cause and is related to autoimmune disorder in which the immune system attacks the thyroid rendering unable to properly produce hormones to control BMR. The link between age and lower thyroid hormone production is a process clinically referred to as hypothyroidism, or an underactive thyroid. Estimated prevalence of subclinical or mild forms of hypothyroidism vary from 5 to 18% among older adults age 60 and older with women being more likely to be diagnosed with thyroid health problems (Diez & Iglesias, 2009; ).
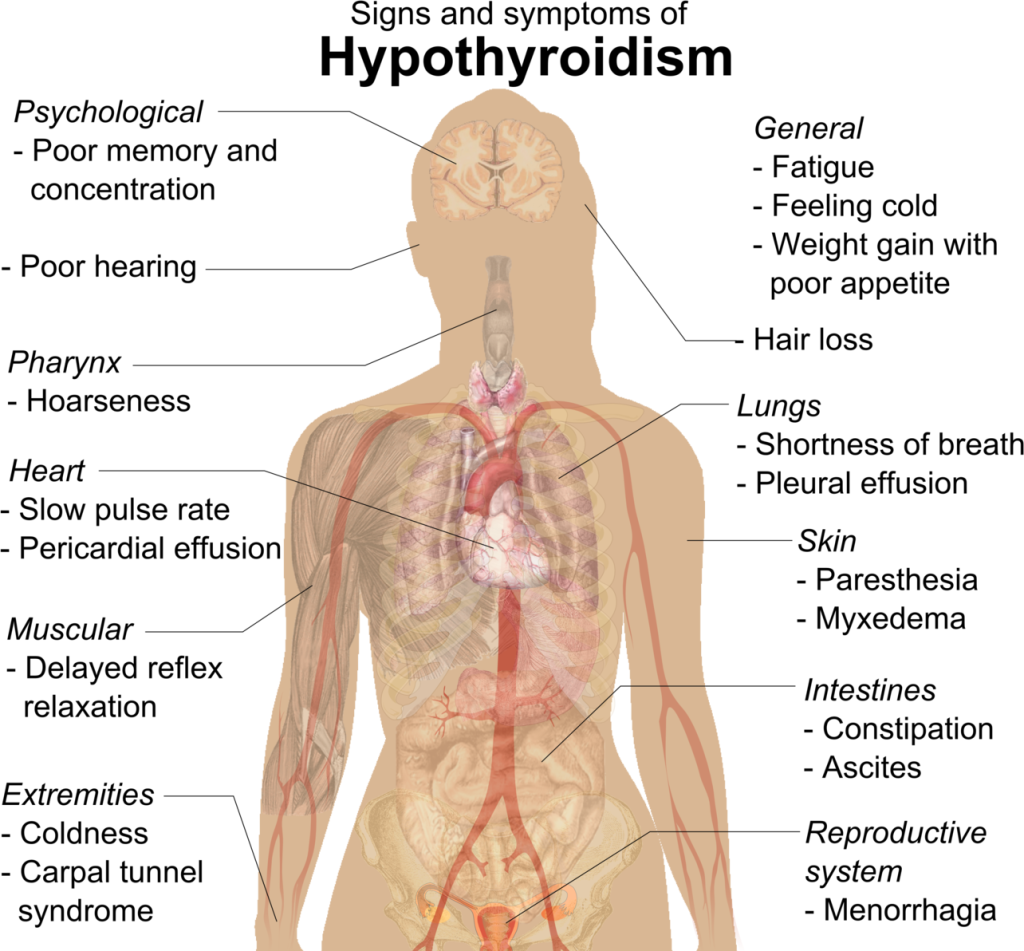

Melatonin
Another hormone, melatonin, is produced by the pineal gland located deep inside the brainstem. Melatonin controls variations in bodily functions associated with sleep and wake cycles, or what is commonly referred to as circadian rhythm. There are significant age-associated differences in circadian rhythm that begin in middle and late adulthood and correspond to the onset and timing of peak melatonin production during the day (Scholtens et al. 2016). Some aging researchers adhere to the belief that melatonin supplements serve as an anti-inflammatory intervention that offsets natural alterations in the hormone, thus contributing to an immunity boost and effectively buffering the risk of contracting viruses as well as the prospect of living with age-associated diseases (Carrillo-Vico et al, 2013; Fvero et al. 2017; Srinivasan et al., 2005; Su et al., 2022). Yet, it is important to recognize that melatonin use can had significant side-effect ranging from migraine headaches, disorientation, drowsiness, and blood vessel constriction. Melatonin supplements can also interfere with sleep cycles if taken at the wrong time of the day or in dosages not aligned with normal circadian rhythms (Vural et al. 2014).
DHEA
The most predominant steroid in the body is dehydroepiandrosterone (DHEA). DHEA is produced by the adrenal glands and is believed to stimulate production of other sex steroids and availability of IGF-1, as well as positively influencing central nervous system functioning. DHEA tends to be higher in males than females with marked decreases of up to 60% across the adult years beginning in age 20 through 80 years of age, a process known as adrenopause. Adrenopause significantly impacts men more than women give higher beginning baseline levels of DHEA. There is a lack of overall evidence to conclude the exact role DHEA plays in human aging with some reports that DHEA replacement therapy is similar to GH and melatonin therapies across anti-aging industrial domains. This has to do with the fact that DHEA present notable health risks in the form of liver functioning problems and prostrate cancer in men (Arnold et al., 2017). More recent evidence suggest that exercise may be the best substitute for any DHEA replacement therapy, noting that physical activity helps compensate for DHEA loss in the latter half of life, especially in men (Al-Turk & Aldujaili, 2016).
Immune System
When gerontologists study stress, they do not just consider major life events, such as unemployment, death of a loved one, or the birth of a child. They are also include metabolic stress, the life sustaining activities of the body, such as circulation ofthe blood, elimination of waste, controlling body temperature, and neuronal firing in the brain. In other words, all the activities that keep the body alive also create biological stress.
To understand how this stress affects aging, problems with the innate and adaptive immune system play a key role. The innate immune system is made up of the skin, mucous membranes, cough reflex, stomach acid, and specialized cells that alert the body of an impending threat. With age these cells lose their ability to communicate as effectively, making it harder for the body to mobilize its defenses. The adaptive immune system includes the tonsils, spleen, bone marrow, thymus, circulatory system and the lymphatic system that work to produce and transport T cells. The human immune system operates to defend bodily health and fight off the noxious effects of stress, acute infections, and potentially lethal threats to our well-being. Immunity operates in sync with the nervous system and therefore influences behavior, perceptions, and emotion (Lupien et al., 2009). The two primary immune cells responsible for protecting human health include “T cells,” and “B cells, which work together with macrophages, a white blood cell that reaches the origin or site of infection via the blood immediately following an attack upon immunity. T-cells are virus or antigen specific, meaning they fight to rid the body of the virus that may be attacking the body. T-cells also come in two forms: (1) Helper T-cells which help coordinate the plan of attack against infection and; (2) Killer T-cells which find and destroy infected cells that have become viral producing. Unlike T-cells, B-cells do not kill antigens themselves. B-cells help sweep-up and clean any leftover viruses after a T-cell attack. Most importantly, B-cells are responsible for the creation of molecules known as antibodies. Antibodies essentially trap invading viruses or other antigens in large clumps making it easy for macrophages to destroy and neutralize infection. Without antibodies, the body would not be able to finish eradicating and ending most infections.
As we continue to age, it is believed that the human body experiences a decline in immune system response and functioning, a process known as immune senescence. In other words, T- and B-cells are negatively impacted by the aging process and lose their ability to effectively protect the body; thus reducing resistance to infections and increasing susceptibility to disease and in some cases morality. Immune senescence was especially apparent during the COVID-19 pandemic, during which over 80% of all COVID-infected deaths occurred among persons aged 65 and older; whereas younger persons may have become infected but did not necessarily die from the disease due to greater natural and biological immunity.
Age-related changes in immunity are believed to be affected by a variety of factors such as diet, exercise, and stress exposure. Investigators have noted that zinc and Vitamin D are two powerful nutrients that can strengthen immune response in later life (Chambers et al., 2021; Maywald & Rink, 2015). Decreases in zinc or vitamin D intake can exacerbate immune senescence. Likewise, deficient protein intake can also be detrimental to immunity in older adults and accelerate spread and severity of infection in the presence of being obese (Garg et al., 2014). However, some experts believe that lifetime patterns of physical movement and moderate to high intensity exercise help to off-set rate of immune senescence in later adulthood (Turner & Braum, 2017). Finally, stress exposure has a deleterious effect on how the immune system is able to ward-off and protect against viral and bacterial infections. Chronic stress can be especially harmful relative to accelerating the rate of aging and contraction of disease. Such processes are further complicated by clinical bouts of anxiety and depression that may be more pronounced after a stressor and increase rates of immune senescence (Vogelzangs et al, 2014).
Reports from immunity studies tend to be highly variable and inconclusive to varying degrees. This reflects a principle known as interindividual variability, or differences in the expression of one or more behaviors or outcomes between members within any given population. Arguments for and against vaccination versus natural immunity surrounding COVID-19 presented a clear example of interindividual variability. Variability relative to who was versus who was not infected, remained asymptomatic, or most at-risk for contracting the COVID-19 virus may have reflected the fact that younger, middle-aged, and older adults maintain different daily lifestyle patterns and routines, sustain various dietary practices, engage in varying levels of exercise intensity, or are impacted uniquely by biological gene activation and expression. This all plays a role in affecting the rates at which one experiences immune system responses and changes, whether COVID is a factor or whatever the virus or bacteria causing an infection may be.
Aging and Nervous System Functioning
The neuronal fallout model has historically been based on the premise that humans progressively lose brain tissue because neurons can no longer replace themselves when they die. This model was largely based on studies that failed to account for a lot of extraneous variables surrounding what happens after death, the methods applied when studying nervous system functioning, and other underlying diseases that contribute to brain tissue loss. More recently, the neuronal fallout model and hypothesis has been gradually debunked by a set of newer more optimistic sources of thinking regarding how the nervous system functions with advancing age. It has become more evident that a plasticity model provides a better examination in which some neurons are highly adaptable and may actually gain in structure and function when other neurons die (Goh & Park, 2009). In fact, the myelination of neuron or the speed with which neurons communicate with each other demonstrate declines in some brain regions but not in others throughout the human life-span (Grydeland et al., 2019). In other words, older adults can demonstrate neural plasticity by compensating for declines in certain brain regions via the activation of other areas that remain in-tact. It is believed that diet, physical activity, aerobic exercise are vital to brain functioning and cognition.
Several contemporary theories have evolved to help explain plasticity of the nervous system functioning involving the brain. Three key theories include:
- Hemispheric Asymmetry Reduction in OLDer adults (HAROLD) Model: the brains of older adult are activated in the opposite hemisphere when the original area suffers a deficit (Maneti et al., 2011)
- Posterior-Anterior Shift with Aging (PASA): the front (anterior) portion of the brain becomes more responsive in order to make up for reduced responsiveness found in the rear or posterior of the brain (Asnado et al., 2012)
- Compensation-Related Utilization of Neural Circuits Hypothesis (CRUNCH) Model: an incorporation of HAROLD and PASA in which it is proposed that the demands of cognitively challenging tasks contributes to increased brain activity in older adults thus leading to compensatory patterns not limited to one particular are but multiple areas (Berlingeri et al., 2013).
Beyond the concept of plasticity in nervous system functioning, the brain maintains a cognitive reserve or untapped resources in the cerebral cortex from which to maintain brain activity and functioning in the presence of deficit. Research indicates that life-long education and learning, challenging occupational tasks or projects, and health-promoting activities help to further build the brain’s capacity to be a reserve of additional resources from which to combat the impact of aging.
Sleep
The human body, mind, and spirit requires sleep for repair, rejuvenation, and healing. It is largely a myth that the older we become, the less sleep we need. Research refutes this notion. It is a fact that all humans, regardless of their age, require 7-9 hours of sleep a night (Ancoli-Israel & Cooke, 2009). Anything less or longer in duration can have adverse health effects ranging from increased stroke risk for women (Waserheil-Smoller et al., 2014) to mental status changes involving anxiety, depressed mood, or memory problems ( ). Studies suggest that good sleep habits play a key role relative to slowing the onset and progression of various chronic disease, most notably Alzheimer’s Disease (Holth et al., 2019; Shokri-Kojori et al., 2018)
Unfortunately, half of all older adults are impacted by sleep disturbances (Neikrug & Ancoli-Israel, 2009). This is largely associated with normative changes in circadian controlling melatonin release and core body temperature which further help regulate sleep cycle. Older adults take longer to fall sleep, awaken more often throughout the night, lie in bed longer and awake before rising, and experience a more shallow and fragmented pattern of sleep (Fetveit, 2009). Such sleep patterns correspond to age alterations surrounding increases in Stage 1 sleep and notable decreases in both Stage 4 and REM (rapid-eye movment) sleep (Kamel & Gammack, 2006). Thus, older adults have higher rates of sleep-wake disorders than their younger counterpart, and they are less able to adjust their sleep patterns under conditions where sleep might be lost such as experiencing jet lag when flying overseas or switching from a day to night shift at work (Duffy et al., 2015). This contribute to noticeable shifts in behavior. For instance, many middle aged and older adults begin to classify themselves as “morning” people thus shifting from a preference to stay up late at night to an adopted preference involving early to bed and early to rise.
Sleep in later life can also be impacted by sleep apnea, a condition in which the individual becomes temporarily unable to breathe while asleep. People who have this condition typically have loud snores followed by silence due to closing of the airway. Respiratory centers of the brain respond to a diminished oxygen intake and the sleeper awakens. This process can occur up to as many as 100 times in a given night. To complicate matters, reduced oxygen in-take forces the heart to pump harder to circulate more blood, which contributes to spikes in blood pressure during the night and elevated blood pressure during the day. Over time, this can contribute an increased risk of hypertension, stroke, arrithymia, and even a heart attack. Sleep apnea is more common among middle aged and older adults who tend to be chronically obese or have a history of diabetes, heart disease or chronic respiratory diseases (Okuro & Morimotu, 2014). However, sleep apnea is very treatable and can be controlled using a continuous positive airway pressure (CPAP device), which keeps the airways open during sleep.
Temperature Control
Many older adults often complain that their sleep is disrupted by an inability to control the feeling of being hot or being cold. Body temperature by itself is an important biological process that impacts health and well-being. Most older adults reside in geographical areas that expose them to variations in climate whether this involve extreme fluctuations in hot temperatures during the summer months or cold and frigid temperatures during the winter months. Older adults are at the greatest risk of dying from two conditions:
- Hyperthermia – a condition in which the human body cannot rid itself of excessive heat or a temperature greatly above normal, including reaching a temperature of 104 and above, which is considered fatalistic to organ and bodily function and;
- Hypothermia – a significant drop in body temperature due to prolonged exposure to cold in which the body is unable to warm up to 95 degrees farenheit or greater.
Together, these two conditions are known as dysthermia. Physiologically, the cause of death under conditions of hypothermia are believed to be due to impaired control of the sympathetic nervous system to constrict the blood vessels in the skin in response to extreme cold temperatures (Greaney et al., 2015). In less extreme conditions, older adults are unable to fully adjust their normal bodily temperature. This is linked to reduced sweat output which causes their core temperature to rise (Dufour & Candas, 2007). In addition, the dermal layer of the skin is much thinner when we are older, thus making it more difficult to cool the skin (Petrofksy et al., 2009). Thus, you may encounter an older adult who feels warm even though the environmental temperature is cold. You may further encounter an older adult who complains of feeling cold despite the environmental temperature being hot. Our ability to control our core temperature diminishes. This creates risk of weather-related death under extreme temperature conditions. In many cases, older adults may reside in a home in which they do not use climate control resources like air conditioning in the summer or heat in the winter.
Aging and Sexual Functioning
It is a myth to think that older adult are not sexually active and concerned about health and functioning when it comes to sexuality. A University of Michigan/American Association of Retired Persons (AARP) poll recently reported that approximately 40% of older adults, aged 65-80, are sexually active. According to the National Institute on Aging (2013), normative age-associated changes in biological functioning can all adversely affect sexual functioning. Hormonal changes, physical disabilities, surgeries, and medicines can also affect and older adult’s ability to participate in and enjoy a healthy sexual relationship. How one feels about sexual intercourse can also affect performance. For example, a woman who is unhappy about her appearance as she ages may think her partner will no longer find her attractive. A focus on youthful physical beauty for women may get in the way of her enjoyment of sex. Likewise, most men have a problem with erectile dysfunction (ED) once in a while, and some may fear that ED will become a more common problem as they age. If there is a decline in sexual activity for a heterosexual couple, it is typically due to a decline in the male’s physical health (Erber & Szuchman, 2015).
There is no doubt that the best way to experience a healthy sex life in later life is to stay sexually active while aging. However, there are clear gender differences when it comes to opportunity for sexual intercourse in later life. The lack of an available partner can affect heterosexual women’s participation in a sexual relationship. Beginning at age 40 there are more women than men in the population, and the ratio becomes 2 to 1 at age 85 (Karraker et al., 2011). Because older men tend to pair with younger women when they become widowed or divorced, this also decreases the pool of available men for older women (Erber & Szuchman, 2015). In fact, a change in marital status does not result in a decline in the sexual behavior of men aged 57 to 85 years-old, but it does result in a decline for similar aged women (Karraker et al., 2011). Thus, older men are more likely to be sexually active with multiple partners compared to older women. This can present health risk for both men and women who are sexually active in old age.
As discussed earlier, normative immune system changes with aging means our bodies become less effective at fighting off illnesses and infections. Symptoms of sexually transmitted infections, such as painful urination, fever, swollen lymph nodes, or sore throat are easy to dismiss as some different type of infection. Yet, the Centers for Disease Control and Prevention (CDC) have reported that STIs have more than doubled among persons aged 65 and old. This largely due to advances in medications that counteract erectile dysfunction for men and vaginal dryness for women. Furthermore, older adults unlike other age groups are least likely to use a condom during sexual intercourse due to the fact there is relatively no risk of pregnancy, particularly when couple is over the age of 65. Therefore, there have been recent efforts to develop new screening instruments that can be used to appropriately educate older adults about sexual activity, the signs and symptoms of transmitted diseases, and how to properly treat any infections should they arise (Smith et al., 2020).
References
Alexandre T., Duarte Y.A.D.O., Santos J., Wong R., Lebrao M. Sarcopenia according to the European Working Group on Sarcopenia in Older People (EWGSOP) versus dynapenia as a risk factor for mortality in the elderly. J. Nutr. Health Aging. 2014;18:751–756. doi: 10.1007/s12603-014-0540-2.
Asher, L. et al. (2012). Most older adults are unable to cross the road in time: A cross-sectional study. Age and Ageing, 41 (5), 690-694. https://doi.org/10.1093/ageing/afs076
Bharucha AE, Dunivan G, Goode PS, et al. Epidemiology, pathophysiology, and classification of fecal incontinence: state of the science summary for the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) workshop. The American Journal of Gastroenterology. 2015;110(1):127–136.
Brown, J.P., Adachi, J.D., Schemitsch, E. et al. Mortality in older adults following a fragility fracture: real-world retrospective matched-cohort study in Ontario. BMC Musculoskelet Disord 22, 105 (2021). https://doi.org/10.1186/s12891-021-03960-z
Boskey, A. L., & Coleman, R. Aging and Bone, Journal of Dental Restoration. 89 (12), 1333-1348. https://doi.org/10.1177%2F0022034510377791
Bouche, P. (2020). Revue neurologique, 176, 9, 733-738. https://doi.org/10.1016/j.neurol.2019.11.007
Cheng, S.T., Fung, H., & Chan, A. (2007). Maintaining self-rated health through social comparison in old age. Journals of Gerontology, Series B, 62(5), P277-P285. https://doi.org/10.1093/geronb/62.5.P277
Christoffersen, M., & Tybjaerg-Hansen, A. (2016). Visible aging signs as risk markers for ishemic heart disease: Epidemiology, pathogenesis, and clinical implications. Ageing Research Review, 25, 24-41. doi: 10.1016/j.arr.2015.11.002.
Dommes, A et al. (2012). Age-related differences in street-cross safety before and after training older adults. Accident Analysis & Prevention, 44(1), 42-47. https://doi.org/10.1016/j.aap.2010.12.012
Faulkner J.A., Larkin L.M., Claflin D.R., Brooks S.V. Age-related changes in the structure and function of skeletal muscles. Clin. Exp. Pharmacol. Physiol. 2007;34:1091–1096. doi: 10.1111/j.1440-1681.2007.04752.x
Giovannini, S. et al. (2021). Neuropathic pain in the elderly. Diagnostics, 11(4), 613. https://doi.org/10.3390%2Fdiagnostics11040613
Hicks, C. W., & Selvin, E. (2019). Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Current Diabetes Report, 19 (10), 86. https://doi.org/10.1007%2Fs11892-019-1212-8
Jerome, G. J. et al. (2015). Gait characteristics associated with walking speed decline in older adults: Results from the Baltimore Longitudinal Study of Aging. Archives of Gerontology-Geriatrics, 60(2), 239-243. https://doi.org/10.1016%2Fj.archger.2015.01.007
Kotronia E, Brown H, Papacosta AO, Lennon LT, Weyant RJ, Whincup PH, Wannamethee SG, Ramsay SE. Oral health and all-cause, cardiovascular disease, and respiratory mortality in older people in the UK and USA. Sci Rep. 2021 Aug 12;11(1):16452. doi: 10.1038/s41598-021-95865-z. PMID: 34385519; PMCID: PMC8361186.
LaCroix AZ, Leveille SG, Hecht JA, Grothaus LC, Wagner EH. Does walking decrease the risk of cardiovascular disease hospitalizations and death in older adults? J Am Geriatr Soc. 1996 Feb;44(2):113-20. doi: 10.1111/j.1532-5415.1996.tb02425.x. PMID: 8576498.
Lorem, G., Cook, S., Leon, D. A., Emaus, N. & Schirmer (2020). Self-reported health as a predictor of mortality: A cohort study of its relation to other health measurements and observation time. Scientific Reports: Nature Research, 10: 4886. https://doi.org/10.1038/s41598-020-61603-0.
Mazur, D. J., & Lipshultz, L, I. (2018). Infertility in the aging male. Current Urology Reports, 17 (19): 54. doi: https://doi.org/10.1007/s11934-018-0802-3
McDaniel C, Ratnani I, Fatima S, Abid MH, Surani S. Urinary Incontinence in Older Adults Takes Collaborative Nursing Efforts to Improve. Cureus. 2020 Jul 12;12(7):e9161. doi: 10.7759/cureus.9161. PMID: 32802599; PMCID: PMC7419143.
- Milsom & M. Gyhagen (2019) The prevalence of urinary incontinence, Climacteric, 22:3, 217-222, DOI: 10.1080/13697137.2018.1543263
- Milsom I, Stewart W, Thuroff J. The prevalence of overactive bladder. The American journal of managed care. 2000 Jul;6(11 Suppl):S565–573.
Ruia S, & Kaufman E. J. (2023). Macular Degeneration. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560778/
O’Sullivan ED, Hughes J, Ferenbach DA. Renal Aging: Causes and Consequences. J Am Soc Nephrol. 2017 Feb;28(2):407-420. doi: 10.1681/ASN.2015121308. Epub 2016 Nov 15. PMID: 28143966; PMCID: PMC5280008.
Sasaki, M. et al. (2018). Gender-specific association of early age-related macular degeneration with systemic and genetic factors in a Japanese population. Scientific Reports, 8, Article: 785 (2018). doi:10.1038/s41598-017-18487-4. https://rdcu.be/diimz
Sayag, M. & Kavé, G. (2022). The effects of social comparisons on subjective age and self-rated health. Ageing & Society, 42(9), 2140-2153. doi: https://doi.org/10.1017/S0144686X20002056
Schuster BG, Kosar L, Kamrul R. Constipation in older adults: stepwise approach to keep things moving. Can Fam Physician. 2015 Feb;61(2):152-8. PMID: 25676646; PMCID: PMC4325863.
Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006;1(3):253-60. doi: 10.2147/ciia.2006.1.3.253. PMID: 18046878; PMCID: PMC2695176.
Shen Y, Huang X, Wu J, Lin X, Zhou X, Zhu Z, Pan X, Xu J, Qiao J, Zhang T, Ye L, Jiang H, Ren Y, Shan PF. The Global Burden of Osteoporosis, Low Bone Mass, and Its Related Fracture in 204 Countries and Territories, 1990-2019. Front Endocrinol (Lausanne). 2022 May 20;13:882241. doi: 10.3389/fendo.2022.882241. PMID: 35669691; PMCID: PMC9165055.
Stamps, J. J., Bartoshuk, L. M., & Heilman, K. M. (2013). A brief olfactory test for Alzheimer’s disease. Journal of Neurological Science, 333, 102, 19-24. https://doi.org/10.1016%2Fj.jns.2013.06.033
Blume-Petyavi, U. et al. (2016). Age-associated skin conditions and diseases: Current perspectives and future options. The Gerontologist, 56 (2), S230=242. https://doi.org/10.1093/geront/gnw003
Rosenberg, I. H. (1997). Sarcopenia: Origins and clinical relevance. Journal of Nutrition, 127, 990S-991s. doi: 10.1093/jn/127.5.990S.
Rudnicka, A. R., Jarrar, Z., Wormald, R., Cook, D. G., Fletcher, A., & Owen, C. G. (2012). Age and gender variations in age-related macular degeneration prevalence in populations of European ancestry: A meta-analysis. Opthalmology, 119,3, 571-580. https://doi.org/10.1016/j.ophtha.2011.09.027
Wuorela, M., Lavonius, S., Salminen, M., Vahlberg, T., Viitanen, M., & Viikari (2020). Self-rated health and objective health status as predictors of all-cause mortality among older people: A prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatrics, 20, Article 120. https://doi.org/10.1186/s12877-020-01516-9
Whitehead WE, Palsson OS, Simren M. Treating fecal incontinence: an unmet need in primary care medicine. North Carolina Medical Journal. 2016;77(3):211–215.
